Importance of Vitreous Retinal Surgery Training
Vitreous Retinal Surgery
The importance of surgical training, trial and error, and continuous improvement to patient
safety and advances in vitreous retinal surgery is well recognized.
The literature agrees that complication rates of experienced surgeons are significantly
lower than beginners and that complications can be devastating.
Given the patient risk and the learning curve,
better training methods are needed in surgical vitreoretinal disease.
Importance of Vitreous Retinal Surgery Training
Although simulation or rehearsal of ocular surgery is desirable, the nature of the eyeball
and its surrounding structures make this a challenging prospect.
Consequently, operating has been the principal means of learning retinal surgery.
It is for these reasons that vitreous retinal surgery has been highlighted as an ideal subspecialty
for training using a virtual reality ocular surgical simulator.
Simulation offers a safe environment where beginners can learn the complex tool manipulation
and tissue dynamics particular to this form of surgery.
By practicing within this environment, it is hoped that surgeons can gain competence
more rapidly and hence reduce the risk to future patients.
Vitreoretinal conditions represent some of the most common and severe causes of visual loss.
Breaks or damage to the retina often result in vitreous traction, which left untreated can cause retinal detachment.
common conditions that require surgery include diabetes-related hemorrhage,
severe inflammation, and complications arising from cataract surgery.
To operate effectively under these conditions, ophthalmologists should receive appropriate training.
Overview of Vitreous Retinal Surgery Techniques
1- Subtotal vitrectomy for retinal detachment: Limited vitrectomy aims to treat the retinal pathology
without inducing further complications and on that basis alone it would be the surgery
of choice for younger patients with rhegmatogenous retinal detachments.
This operation spares the vitreous base and removes mainly the anterior
and mid vitreous without posterior hyaloid separation.
2- Posterior vitreous detachment: This surgical option may be advised for symptomatic PVD
with a large tear and retinal detachment occurring at the time of floaters and flashing lights.
Too frequently the retinal symptoms have led to vitrectomy being performed before adequate PVD has occurred.
Surgical Techniques in Vitreous Retinal Surgery
The training is based on explaining Surgical Techniques in Vitreous Retinal Surgery and how to perform each of them:
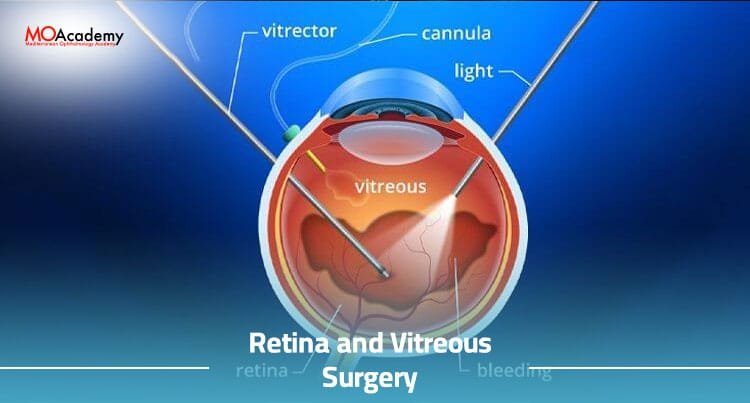
Pars plana vitrectomy (PPV) refers to a particular method of removing the vitreous from the eye.
The vitreous is removed because it has caused problems within the eye, such as a retinal detachment or bleeding.
In a standard PPV, the surgeon makes three incisions in the eye: one into the white part of the eye
and two where the iris meets the white part of the eye.
The surgeon will then connect a tube to the center incision and remove the vitreous.
The advantages of this method are it involves less trauma to the eye than previous vitrectomy
methods and most of the instruments remain within the eye and are not visible externally,
so there is less of an intimidation factor for the patient.
There are several techniques used to repair a retinal detachment.
The method chosen depends on what extent the detachment has progressed.
If the detachment is still in the early stages and is only secondary to a retinal tear,
then often the best method is to create a chorioretinal adhesion around the tear using cryopexy or laser.
This method can be performed in an outpatient clinic. If the detachment is more severe,
then an operation involving a vitrectomy will be required.
This is often the case when the detachment is caused by scar tissue that has contracted and pulled the retina off.
This method can take several forms, one such option is that during the removal of the vitreous,
the surgeon uses a small pick to gently lift the retina back into position.
A second method involves placing perfluorocarbons (gases) or silicone oil into the eye
to push the retina back in place after the vitrectomy has been completed.
The use of PPV in conjunction with modern techniques means that the success rate for retinal
detachment has vastly improved.
Practical Training in Vitreous Retinal Surgery
Trainees may not have had the opportunity to perform VR surgery during their residency.
Likewise, the complex nature of the surgery may mean that a trainee is not confident
enough to attempt a particular procedure.
The difficulties in obtaining surgical experience make it difficult for a beginner
to progress to a competent vitreous retinal surgery
1- Hands-on Surgical Experience
The wet lab course Instructional techniques include didactic lectures, one-on-one teaching
with the course instructors, and the use of surgical simulators.
Lecture topics cover basic and advanced techniques for repairing complex retinal detachment,
repair of proliferative vitreoretinopathy, endophthalmitis, and repair of complex macular pathology.
Commonly used instruments employed for these techniques are also reviewed in detail.
After attending this course, one should have a comprehensive understanding of the techniques
and instrumentation needed to perform a vitreoretinal surgical repair.
A properly equipped wet lab offers an environment where a student can work with vitreous
and retina under excellent visualization.
This type of setting provides the best possible situation for learning how to perform a vitreoretinal surgical technique.
2- Observation of Experienced Surgeons
Trainees must also be allowed to observe experienced surgeons in a clinical setting.
Clinical observation has always been a valuable learning tool in surgery and has been shown
to improve patient outcomes.
However, with recent changes in resident work hours and the tempo of modern vitreoretinal surgery,
attending surgeons may find it difficult to engage trainees in operative settings.
High patient acuity, complex surgical cases, and the risk of medical errors have placed
increased stress on attending surgeons and operating room staff.
Operative teaching often slows down the surgery and puts the patient at risk.
Busy surgeons may avoid teaching cases altogether.
These factors have created an increasingly hostile environment for clinical teaching during live surgery.
Vitreous Retinal Surgery Training Program at MoAcademy
- Didactic Training Sessions
- Hands-on Surgical Training
- Observation and Assistance in Real Surgeries
- Case Studies and Surgical Decision-making